Medical Billing vs. Revenue Cycle Management: What’s The Difference?
First, we will focus on medical billing. Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for healthcare services provided to patients. It serves as the base of financial transactions in the healthcare space. Its main purpose is to ensure that the services provided by doctors are accurately documented and paid for.
Claim Generation:
This is the start of the medical billing process. This step is where the claim is created. After a doctor provides a service to a patient, the claim is translated into different codes that are recognized by insurance companies and government payors. This involves coding using systems such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT).
Claim Submission:
Once the claims are generated, they are sent to the payers or private insurers, such as Medicare or Medicaid. This step involves adhering to strict guidelines and timelines. In New York State, claims for any medical care or service must be sent within 90 days (about 3 months) of the date of service.
Payment Posting:
As payments are received from payers, they are recorded in the provider’s medical billing system. This includes payments, denials, and any adjustments that may need to be made. This step requires accuracy and attention to detail.
Follow-Up:
In specific scenarios where claims may be denied or need adjusting, this is a very crucial step. Following up is crucial to make sure that both the payer and provider secure the right payment. This step may involve appeals, the need for additional documents, and the addressment of any coding errors. It is always important for providers to maximize revenue.
Patient Registration:
Receptionists should be (1) ensuring that the patient goes through a seamless registration process, (2) verifying the patient’s insurance and (3) be estimating the patient’s financial responsibility before they even walk through the door.
Charge Capture:
This step focuses on capturing all billable services provided to the patient. This step helps the provider minimize revenue leakage from missed charges or coding errors. This step is like Step 1 of the medical billing process.
Claim Submission:
Once all the services are coded and documented, claims are sent to the insurance companies. RCM systems usually include features such as electronic claim submission, which speeds up the payment process. This step is like Step 2 of the medical billing process.
Payment Posting & Billing:
Once the insurance payments are received, they are transferred to the patient’s account in the RCM system. After all the insurance payments are processed, the patient is billed for any remaining expenses. RCM systems generate financial statements and manage the billing process, including following up with any unpaid balances.
Denials and Follow Ups:
If a claim is denied by an insurance payor, the RCM staff must get involved and investigate the reason as to why. They then appeal and solve the issue. Finally, if there are still any unpaid patient balances, the RCM staff may have to set up payment plans or negotiate settlements.
Start of the CRM process
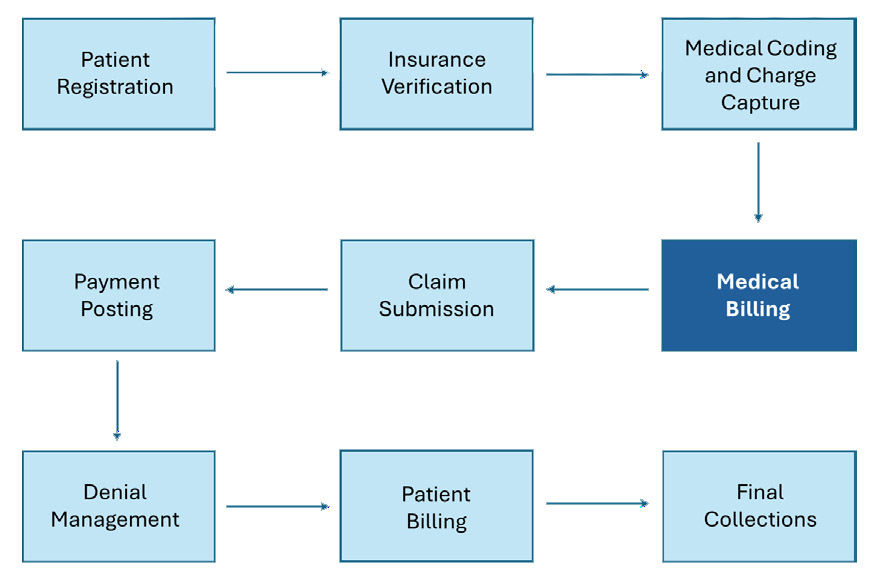
End of the CRM process
Interested in Learning More?
We would love to hear from you! Please reach out to us