The Evolution of Revenue Cycle Management in Healthcare
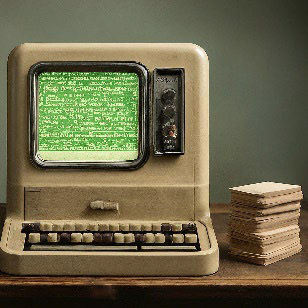
The 1970s marked a turning point with the arrival of computer technology. Early RCM software developed claim processing and introduced standardized billing codes, improving communication with insurers and boosting reimbursement rates.
In 1996, the Health Insurance Portability and Accountability Act (HIPAA) was introduced. This act mandated standardized electronic billing practices, making RCM more efficient and clearer for private practices and introducing the concept of “covered entities” responsible for safeguarding patient data electronically.
Today’s healthcare landscape prioritizes value-based care, rewarding providers for high-quality care. This shift has made RCM even more critical; healthcare organizations now require a broader range of metrics to demonstrate quality care delivery.
Another contemporary trend is the growing patient financial responsibility. Patients are demanding transparency in pricing. This necessitates prioritizing price transparency, making it easier for patients to understand potential costs.

Interested in Learning More?
We would love to hear from you! Please reach out to us